11 - 12 November 2025 | Crowne Plaza, Auckland
Innovation and Excellence in Primary and Community Care
Building a stronger health system from the ground up
Innovation & Excellence in Primary & Community Care 2025 is where New Zealand’s health transformation begins.
This conference will support the shift from hospital-centric, episodic care to an integrated, community-based, and prevention-focused health system. Through sharing local best practices, global policy, and new technologies, the event provides a crucial roadmap for operational excellence and service expansion to meet the needs of our changing communities.

Key themes for 2025 include:
Future-Focused Care Models & Policy
● Explore the latest in primary care policy, including funding changes and the deployment of transformative technologies like AI and telehealth. Discover how PHOs are driving health system transformation through innovation and integrated care models.
Workforce & Service Excellence
● Learn how to invest in and develop future workforces for primary, community, and rural care. The event will showcase strategies for achieving provider business excellence, service diversification, and effective business management.
Population Health & Case Studies
● Understand the critical role of primary care in tackling population health determinants and providing optimal care. The conference will highlight compelling case studies of excellence and innovation across all sectors, including rural, urgent, and after-hours care.
Innovation & transformation
● Primary and community care innovation and transformation policy and primary care funding change
Future workforce & care models
● Investing in primary care, community and rural workforces and exploring future workforce models and associated models of care
PHO deep dive
● How PHOs are driving health system transformation by testing, scaling and deploying primary care innovations
AI, Telehealth, Technology
● Deploying transformative technology innovations in primary care including AI and telehealth
Tackling health determinants
● The role of primary care in supporting population and public health approaches to tackling health determinants
Case studies of excellence
● Showcasing case studies of innovation and excellence from across the spectrum of primary care, community services and urgent care
Achieving provider business and service excellence
● Excellence and innovation in primary and community health provider business management and general practice service innovation and diversification
Integrated care and system redesign
● The critical role of primary care in whole system redesign focusing on care integration and coordination – ensuring right care, in the right place, at the right time
Rural Urgent Unplanned Care (RUUC)
● Delivering future visions for Urgent and After Hours and Rural Urgent Unplanned Care
Key themes for 2025 include:
- Primary and community care innovation and transformation policy and primary care funding change
- Investing in primary care, community and rural workforces and exploring future workforce models and associated models of care
- How PHOs are driving health system transformation by testing, scaling and deploying primary care innovations
- The critical role of primary care in whole system redesign focusing on care integration and coordination – ensuring that patients receive the right care, in the right place, at the right time
- The role of primary care in supporting population and public health approaches to tackling health determinants
- Showcasing case studies of innovation and excellence from across the spectrum of primary care, community services and urgent care
- Excellence and innovation in primary and community health provider business management and general practice service innovation and diversification
- Deploying transformative technology innovations in primary care including AI and telehealth
- Delivering future visions for Urgent and After Hours and Rural Urgent Unplanned Care
KEY SPEAKERS FOR 2025
Our 2025 lineup brings together leading practitioners, private and public thought leaders in primary healthcare.
Check out more today.

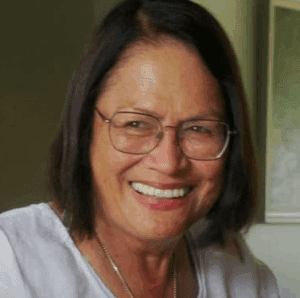
Kim Sinclair-Morris
Chief Executive Officer | Manukura
Pegasus Health

Dr Andy Knox MBE
Medical Director
NHS Lancashire and South Cumbria Integrated Care Board

Dr Fiona Bolden
Chair
Hauora Taiwhenua | Rural Health Network
Add Your Heading Text Here

Sub Heading Here
Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.Lorem ipsum dolor sit amet
Sub Heading Here
Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.Lorem ipsum dolor sit amet

Sub Heading Here
Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.Lorem ipsum dolor sit amet

Sub Heading Here
Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.Lorem ipsum dolor sit amet
Add Your Heading Text Here
We are currently working on the programme and agenda.
If you would like to have input into our research programme please email xxxx@brightstar.co.nz
Add Your Heading Text Here
Sub-heading
Date or content
Sub-heading
Date or content
Sub-heading
Date or content
Sub-heading
Date or content
Sub-heading
Date or content
Venue
The location and how you can get there
Address
Crowne Plaza Auckland by IHG
128 Albert Street, Acukland Central 1010
Agenda
Agenda to be announced
8:50 | Registration and Coffee |
9:00 | Mihi whakatau |
9:00 | Welcoming remarks from Conference Chair |
9:10 | Reaffirming the core role of primary care and General Practice in meeting the health needs of New Zealanders
Hon Simeon Brown, Minister of Health, Minister for State Owned Enterprises, Minister for Auckland (remote presentation) |
9:40 | Primary care workforce development, innovation and transformation
|
10:30 | Morning break |
11:00 | Panel discussion: How can we better drive health system transformation through primary and community care innovation
Kim Sinclair-Morris, Chief Executive Officer | Manukura, Pegasus Health Paul Roseman, General Manager Strategic Development, ProCare Dr Jeff Lowe, Partner & Specialist GP, Karori Medical Centre Jess Morgan-French, CEO, Collaborative Aotearoa Dr Bryan Betty, Chair, GPNZ |
11:40 | Enabling digital access to 24/7 primary care
|
12:20 | Lunch |
1:20 | Using primary care innovation as the building block for health and care system transformation through the delivery of effectively coordinated care services
Professor Nick Goodwin, Visiting Professor - Centre for Research in Health System Performance (CRiHSP), National University of Singapore |
2:00 | Case study: Coordinating integrated care for high needs older people with multi-morbidly in primary care
Dr Katherine Bloomfield, Senior Lecturer - Department of Medicine, University of Auckland and Geriatrician, Te Whatu Ora Waitemata |
2:40 | Case study: Delivering population and public health interventions in primary care to tackle health determinants
Dr Andy Knox MBE, Medical Director, NHS Lancashire and South Cumbria Integrated Care Board, Associate, Centre for Population Health, Co-Founder, Population Health Leadership Academy, GP Partner, Ash Trees Surgery & Honorary Professor, Lancaster University Management School (UK) |
3:20 | Afternoon break |
3:40 | Delivering primary care innovation to better meet the needs of Māori and Pacific communities
Boyd Broughton, Chief Executive Officer, Te Taumata Hauora o Te Kahu o Taonui Iwi Māori Partnership Board |
4:20 | Case study: Empowering communities through the provision of kaupapa Māori primary care
Lady Tureiti Moxon, Chief Executive, Te Kōhao Health |
5:00 | Summary remarks from the Chair & Networking Drinks |
9:00 | Welcome back from Conference Chair |
9:05 | Analysing changing general practice ownership models
|
9:50 | Excellence and innovation in primary and community health provider business management
Jess Morgan-French, Chief Executive, Collaborative Aotearoa |
10:30 | Morning break |
11:00 | General practice service innovation and diversification – expanding the suite of services practices provided to patients
|
11:30 | Case study: Delivering Primary Options for Acute Care (POAC) - ensuring patients receive the right care, in the right place, at the right time
|
12:00 | Using AI tools in general practice and primary care
|
12:30 | Developing a next-level patient portal to enable the delivery of connected patient-centred care
|
1:00 | Lunch and networking |
2:00 | Delivering the Urgent and After-hours Framework – investing in improving access to urgent and after-hours healthcare services across New Zealand
Dr Jasmine Mackay, Clinical Director, 24 Hour Surgery |
2:30 | A vision for the future system of rural urgent unplanned care
Dr Fiona Bolden, Chair, Hauora Taiwhenua | Rural Health Network |
3:00 | Innovation in the management of mental health in primary care
|
3:30 | Summary remarks from the Chair & end of Conference |
Speakers
Speakers to be announced
Lady Tureiti Moxon
Read bio

Dr Bryan Betty
Read bio

Hon Simeon Brown
Read bio

Dr Jeff Lowe
Read bio

Dr Fiona Bolden
Read bio

Dr Katherine Bloomfield
Read bio

Boyd Broughton
Read bio

Paul Roseman
Read bio

Professor Nick Goodwin
Read bio

Dr Andy Knox MBE
Read bio

Jess Morgan-French
Read bio

Dr Matthew Wright
Read bio
Don't miss out on the connections and credibility boost!
Live B2B events are your chance to shine. Showcase your thought leadership, solidify your market position, and forge valuable connections with potential customers – all at once.
This exclusive event puts you in front of a highly skilled audience hungry for insights. Get ready for meaningful engagement that drives results.
Plus, we have some unique opportunities to put your company, products, and services in the spotlight.
Ready to take your brand to the next level? Contact us today to learn more or secure your spot at this leading event.

Practice rate tickets
Must be from a general practice, urgent care provider or be a practice manager.
Practice rate ticket
- Early Bird
-
Must be from same organisation and book at same time. For valid ticket/s, payment by 17 October, 2025.
Practice rate ticket
- Last Minute
-
Must be from same organisation and book at same time. For valid ticket/s, payment by 11 November, 2025.
Standard
Registration Conditions
Ticket Terms
All prices are in New Zealand dollars ($NZD)
A surcharge of 2.5% + GST applies to credit card payments on top of the total amount.
Pre-Sale Tickets are valid only for the specific event for which they were purchased and cannot be transferred to other events. To remain valid, Super Saver and Early Bird tickets must be paid by date quoted.
Group ticket options are valid for registrations from the same organisation, booked at the same time.
By selecting any special pricing offer for classes of organisation, sector, or individuals or using any promotion code, you are asserting to the organiser your right to claim any such pricing offer, and acknowledge the organiser’s right to audit such claim and, if in the opinion of the organiser using its sole discretion the conditions for special pricing are not met, reject any registration.
For full terms & conditions, please visit https://www.brightstar.co.nz/terms-and-conditions
Make an enquiry
Got questions? Write to us.



